Candida, Clostridia, and the Gut–Brain Axis
The Effects on Mood, Brain Fog, and Mental Health
By Dr. Alain Frabotta - Integrative Chiropractor, Naturopathic & Functional Medicine Clinician, Educator, Sydney, Australia, integrating nutritional, lifestyle, and genomic medicine into modern clinical care.
Executive Summary
The human gut is home to trillions of microorganisms—including bacteria, fungi, viruses, and archaea—that collectively form the gut microbiome [1,2].
Over the past two decades, advances in microbiology, immunology, and neuroscience have demonstrated that this microbial ecosystem plays a meaningful role in brain health through the microbiota–gut–brain axis, a bidirectional communication network linking the gastrointestinal tract and the central nervous system [1–4].
Two microbial groups that have received particular attention in this context are Candida (a genus of yeast) and Clostridia (a diverse class of anaerobic bacteria). Both are normal components of the human gastrointestinal ecosystem and often exist without causing disease [5,6].
Clinical relevance emerges when microbial balance is disrupted—a state referred to as dysbiosis—allowing certain Candida species or toxin-producing Clostridia to proliferate disproportionately [6–8].
Under dysbiotic conditions, these organisms may influence neurological and psychological function through several interrelated mechanisms, including intestinal barrier disruption, immune activation, inflammatory signalling, altered microbial metabolite production, and modulation of neurotransmitter pathways [1,3,9–11].
Accumulating evidence links gut dysbiosis involving Candida and Clostridia to symptoms such as fatigue, impaired concentration, mood disturbances, anxiety, and—more controversially—to neurodevelopmental and neuropsychiatric conditions [3,9,12–15].
Although causality is not always established, understanding how Candida and Clostridia interact with the gut–brain axis provides a biologically plausible framework for appreciating how gastrointestinal health may shape mental and cognitive well-being.
1. The gut microbiome and the brain
1.1 The gut–brain axis
The gut–brain axis refers to the bidirectional communication network linking the gastrointestinal tract and the central nervous system through neural, immune, endocrine, and metabolic pathways [1–4]. Key components of this system include:
The vagus nerve and enteric nervous system [2,3]
The immune system, particularly gut-associated lymphoid tissue (GALT) [4,9]
Neuroendocrine pathways, including the hypothalamic–pituitary–adrenal (HPA) axis [10,11]
Microbial metabolites, such as short-chain fatty acids, amino-acid derivatives, and inflammatory mediators [9,16–18]
Signals originating in the gut influence mood, cognition, stress responsiveness, and behaviour, while psychological stress and neurological disease can, in turn, alter gut motility, permeability, immune tone, and microbial composition [2,10,11].
Large population studies, translational research, and animal models demonstrate that disruptions in the gut microbiome are associated with depression, anxiety disorders, neurodevelopmental conditions, neurodegenerative diseases, and age-related cognitive decline [1,3,12,19–21].
Candida and Clostridia exemplify how specific microbial groups can influence brain health both indirectly—through immune and metabolic signalling—and, in rare cases, more directly via neuroactive toxins or inflammatory responses [6,9,14,22].
2. Candida: a common yeast with complex effects
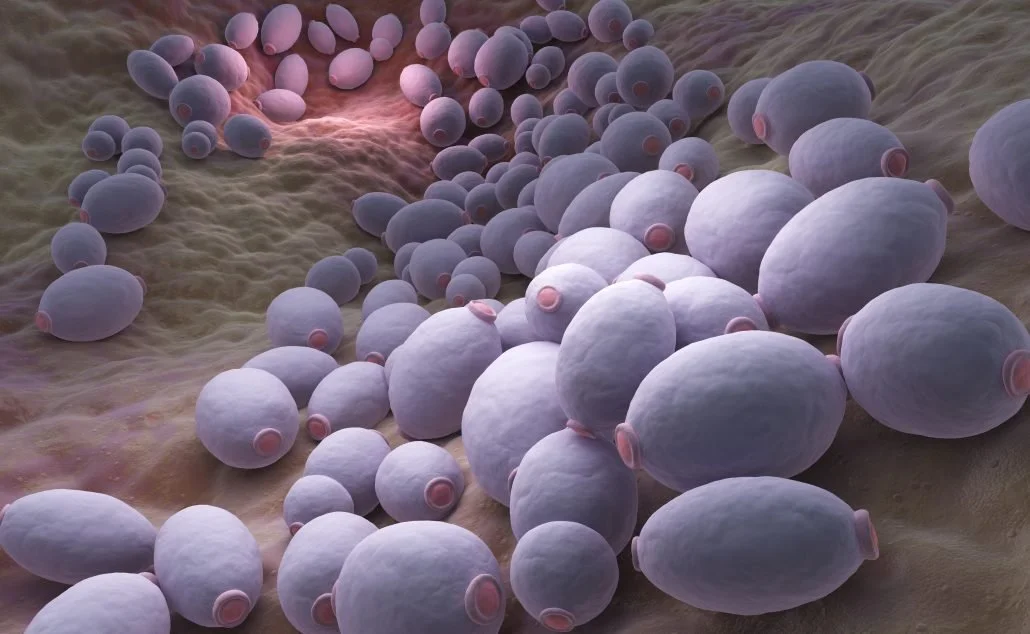
Candida species are fungi that form part of the normal human mycobiome, with Candida albicans being the most extensively studied [12,23].
In healthy individuals, Candida exists in low abundance and is regulated by host immunity and bacterial competitors, particularly Lactobacillus species [23,24].
Under conditions such as antibiotic exposure, immune dysregulation, or chronic intestinal inflammation, Candida can shift from a benign yeast form into an invasive filamentous phenotype, increasing its capacity to disrupt epithelial barriers and activate immune pathways [12,25–27].
2.1 Candida as a normal gut resident
Candida species are commensal fungi that form part of the normal human mycobiome, with Candida albicans being the most extensively studied species [12,23]. Low-level Candida colonisation of the oral cavity, gastrointestinal tract, and genitourinary mucosa is common and typically asymptomatic in immunocompetent individuals [23,24].
Under healthy conditions, Candida growth is constrained by multiple host and microbial factors, including intact mucosal barriers, innate and adaptive immune surveillance, and competitive inhibition by commensal bacteria—particularly Lactobacillus and Bifidobacterium species [24–26]. In this balanced state, Candida exists predominantly in a unicellular yeast form and contributes to microbial diversity without inducing inflammation or tissue damage [23,27].
2.2 When Candida becomes problematic
Candida becomes clinically relevant when ecological balance within the gut is disrupted, allowing excessive proliferation or phenotypic switching. Common predisposing factors include:
Broad-spectrum or repeated antibiotic exposure [26,28]
Immune dysregulation or suppression [27,29]
Chronic intestinal inflammation and barrier dysfunction [12,30]
Sustained physiological stress and altered cortisol signalling [31]
Under these conditions, C. albicans can transition from its yeast form into an invasive filamentous (hyphal) phenotype, which enhances adhesion to epithelial cells, tissue penetration, and immune activation [25,27,32]. This morphological shift represents a key virulence mechanism and distinguishes benign colonisation from pathogenic behaviour [25,32].
2.3 Candida and intestinal permeability
A growing body of experimental and translational evidence indicates that Candida overgrowth can contribute to increased intestinal permeability [12,30,33]. Hyphal Candida expresses adhesins and secreted proteases capable of disrupting tight junction proteins and degrading the protective mucous layer of the intestinal epithelium [25,30].
Barrier disruption allows translocation of fungal antigens (e.g. β-glucans and mannans), bacterial products, and inflammatory mediators into systemic circulation, amplifying immune activation beyond the gut [30,34]. This process has been implicated in fatigue, malaise, and cognitive symptoms associated with chronic inflammatory states [9,33,35].
Importantly, increased permeability does not imply invasive fungal infection; rather, it reflects altered host–microbe interactions that can influence distant organs, including the brain, through immune and metabolic signalling pathways [1,9].
2.4 Candida-derived metabolites and brain effects
Candida species produce several metabolic by-products with potential neurobiological relevance, particularly in the context of dysbiosis and impaired detoxification pathways. These include:
Acetaldehyde, a toxic intermediary of ethanol metabolism that interferes with neurotransmitter synthesis and mitochondrial energy production [36,37]
Ammonia, which can alter neuronal excitability and contribute to mental fatigue [38]
Secondary fungal metabolites capable of modulating immune responses and oxidative stress [39]
Acetaldehyde is of particular interest because it can cross the blood–brain barrier and disrupt dopamine, serotonin, and glutathione metabolism [36,37]. Experimental data and clinical observations suggest that elevated acetaldehyde exposure may contribute to symptoms commonly described as “brain fog,” headaches, impaired concentration, and reduced cognitive clarity, although these manifestations are typically multifactorial [35–37].
It is critical to note that these mechanisms are most relevant when Candida overgrowth coexists with impaired barrier integrity, altered hepatic detoxification capacity, or high inflammatory burden, rather than in isolated low-level colonisation [12,30,35].
2.5 Candida, stress physiology, and neuroendocrine signalling
Beyond immune and metabolic effects, Candida may influence the brain through neuroendocrine pathways.
In a landmark experimental study, gut colonisation with Candida albicans in adolescent mice—without systemic infection—was associated with increased anxiety-like behaviour and elevated stress hormone levels [40].
Mechanistically, these effects were mediated through alterations in the endocannabinoid system, a key regulator of emotional behaviour, stress responsivity, and hypothalamic–pituitary–adrenal (HPA) axis activity [40,41].
Pharmacological enhancement of endocannabinoid signalling reversed both behavioural and neuroendocrine abnormalities, providing strong evidence for a gut-derived signalling mechanism rather than direct neural infection [40].
While these findings cannot be directly extrapolated to humans, they establish biological plausibility for Candida-associated modulation of stress and mood regulation through gut–brain communication pathways [3,10,40].
2.6 Clinical interpretation
From a clinical standpoint, Candida is best understood not as a universal cause of neuropsychiatric symptoms, but as a potential contributing factor in a subset of individuals with:
Co-existing gastrointestinal symptoms
Antibiotic-associated dysbiosis
Chronic inflammatory or stress-related conditions
In such contexts, Candida-related barrier disruption, immune activation, and neuroendocrine modulation may amplify existing vulnerability rather than independently drive disease [12,35,42].
3. Clostridia: beneficial bacteria and potential pathogens (inline-cited)
3.1 Understanding Clostridia in the human gut
Clostridia refers to a large and phylogenetically diverse class of anaerobic, spore-forming bacteria within the Firmicutes phylum [19,20]. Importantly, Clostridia are not a single organism and should not be regarded as uniformly harmful. In fact, many Clostridial species are essential contributors to gut health, immune regulation, and metabolic homeostasis [19–21].
Several commensal Clostridia clusters—particularly clusters IV and XIVa—play a central role in fermenting dietary fibre into short-chain fatty acids (SCFAs), including butyrate, acetate, and propionate [20–22].
These metabolites support intestinal epithelial integrity, promote regulatory T-cell differentiation, and contribute to immune tolerance within the gut [21–23]. Through these mechanisms, beneficial Clostridia indirectly support brain health by maintaining barrier function and limiting systemic inflammation [1,9,21].
3.2 Pathogenic and toxin-producing Clostridia
In contrast to commensal species, some Clostridia are clinically significant pathogens, particularly when microbial balance is disrupted. These include:
Clostridioides difficile, a leading cause of antibiotic-associated colitis [37,38]
Clostridium perfringens, capable of producing multiple exotoxins [22,39]
Clostridium botulinum and Clostridium tetani, producers of potent neurotoxins [39]
While classic neurotoxins such as botulinum and tetanus toxins are typically associated with acute, severe infections, other Clostridial species produce metabolites that may exert subtle but chronic neurobiological effects when present in excess or in susceptible hosts [19,22,40].
3.3 Antibiotics, dysbiosis, and Clostridial overgrowth
Antibiotic exposure is a well-established risk factor for Clostridial dysbiosis [26,37]. By reducing microbial diversity and eliminating competitive bacterial species, antibiotics create ecological niches that allow resistant Clostridia—particularly C. difficile—to proliferate [37,38].
Clinically, C. difficile infection is associated not only with diarrhoea and colitis, but also with fatigue, delirium, and cognitive dysfunction, especially in older adults [38,41]. These neurological manifestations are thought to reflect systemic inflammation, metabolic stress, and cytokine-mediated effects on the brain rather than direct neuroinfection [41,42].
3.4 Clostridial metabolites and neurotransmitter pathways
Beyond acute infection, certain Clostridia are capable of producing phenolic and aromatic metabolites with potential relevance to brain function. Of particular interest are:
p-cresol and p-cresyl sulfate, derived from tyrosine metabolism
4-hydroxyphenylacetic acid, derived from phenylalanine metabolism
These compounds can cross the intestinal barrier—especially when permeability is increased—and enter systemic circulation [11,43]. Experimental studies demonstrate that p-cresol can interfere with catecholamine metabolism by inhibiting dopamine-β-hydroxylase, altering dopamine and norepinephrine balance [11,44].
Animal models further show that p-cresol exposure can induce anxiety-like behaviour, social impairment, and repetitive behaviours, supporting a biologically plausible link between microbial metabolite burden and neurobehavioural changes [11,45].
In humans, elevated urinary or plasma p-cresol levels have been reported in subsets of individuals with neurodevelopmental and neuropsychiatric conditions, though findings are heterogeneous and not universally present [5,11,46].
3.5 Short-chain fatty acids: neuroprotection versus imbalance
SCFAs represent one of the most important classes of microbial metabolites involved in gut–brain communication [9,16]. Butyrate, in particular, has anti-inflammatory and neuroprotective properties, supporting blood–brain barrier integrity and modulating microglial maturation [20,21,47].
However, animal models suggest that excessive propionate exposure, especially during critical periods of neurodevelopment, may induce neuroinflammatory responses and behavioural abnormalities [45,48].
These findings do not imply that SCFAs are harmful per se, but rather that metabolic balance and microbial diversity are critical determinants of their net effect on brain health [16,21].
3.6 Clostridia and neurodevelopmental research
Clostridia have been extensively studied in relation to autism spectrum disorder (ASD), particularly in individuals with prominent gastrointestinal symptoms. Early microbiological studies identified increased abundance and diversity of Clostridial species in stool samples from children with regressive autism compared with controls [5,49].
Subsequent clinical observations noted that oral vancomycin—poorly absorbed and active against anaerobes—was associated with temporary improvements in behavioural symptoms in some children, suggesting a microbiome-mediated effect rather than direct neurological action [5,49].
More recent microbiota-based interventions, including structured microbiota transfer protocols, have demonstrated sustained improvements in gastrointestinal symptoms and modest improvements in behavioural measures in open-label studies [6,7,50].
These findings support a modulatory role for Clostridia-related dysbiosis in a subset of individuals with ASD, while falling short of establishing causality [6,7,46].
3.7 Clinical interpretation
From a clinical perspective, Clostridia should be viewed as a functionally diverse group, encompassing both essential commensals and opportunistic pathogens. The goal of intervention is therefore not eradication, but restoration of microbial balance and metabolic harmony [19–21].
In individuals with gastrointestinal symptoms, antibiotic exposure, or inflammatory comorbidities, Clostridial dysbiosis may contribute to neuropsychiatric symptom burden through immune activation and metabolite-mediated effects [9,41,42]. In asymptomatic individuals, however, Clostridia remain a vital component of a healthy gut ecosystem.
6. Neuropsychiatric and cognitive associations
6.1 Brain fog, fatigue, and cognitive symptoms
“Brain fog” is not a formal diagnostic entity but a widely reported constellation of symptoms that includes impaired concentration, slowed information processing, memory lapses, and mental fatigue. These symptoms are commonly reported in chronic inflammatory states and functional gastrointestinal disorders and are increasingly examined through a gut–brain axis framework [9,12,35,51].
In the context of Candida or Clostridial dysbiosis, several overlapping mechanisms may contribute to cognitive symptoms:
Systemic immune activation and cytokine signalling affecting central neurotransmission [9,43,52].
Oxidative stress and mitochondrial dysfunction, potentially exacerbated by microbial metabolites such as acetaldehyde and phenolic compounds [36,37,44]
Altered neurotransmitter synthesis and metabolism, particularly involving dopamine and serotonin pathways [11,36,53].
Sleep disturbance secondary to gastrointestinal symptoms, which independently impairs cognitive performance [51,54].
Importantly, these symptoms are typically multifactorial. Gut dysbiosis may act as a contributing or perpetuating factor rather than a primary cause, particularly in individuals with pre-existing metabolic, inflammatory, or psychological vulnerability [12,35,51].
6.2 Anxiety and stress-related disorders
Anxiety disorders are closely linked to dysregulation of the stress response system, including the hypothalamic–pituitary–adrenal (HPA) axis, autonomic nervous system, and inflammatory signalling pathways [10,11,55].
The gut microbiome has emerged as a key modulator of these systems [1,3,10].
Experimental studies demonstrate that alterations in gut microbial composition can influence anxiety-like behaviour through immune, vagal, and neuroendocrine pathways [3,10,55].
Candida-specific animal research has shown that Candida albicans colonisation can alter stress hormone regulation and anxiety-related behaviour via disruption of the endocannabinoid system, providing a mechanistic link between fungal dysbiosis and stress physiology [40,41].
In humans, anxiety disorders are associated with altered gut microbiome diversity and increased markers of intestinal permeability and inflammation [55–57].
While Candida and Clostridia are unlikely to be singular drivers of anxiety, they may amplify stress sensitivity and symptom severity in susceptible individuals, particularly those with co-existing gastrointestinal complaints [12,55].
6.3 Depression and mood disorders
Major depressive disorder is increasingly recognised as a systems-level condition, involving immune activation, altered tryptophan metabolism, HPA-axis dysregulation, and changes in neuroplasticity [52,58]. Large-scale studies and meta-analyses have identified consistent associations between depression and gut microbiome alterations, including reduced microbial diversity and shifts in metabolite profiles [3,52,59].
Microbial influences on depression may operate through several pathways relevant to Candida and Clostridia:
Inflammatory cytokine signalling, which can reduce monoamine availability and impair neurogenesis [52,58].
Altered tryptophan metabolism, favouring the kynurenine pathway over serotonin synthesis during chronic immune activation [53,58].
Reduced short-chain fatty acid production, impairing barrier integrity and immune regulation [16,21,59].
Clinical trials investigating probiotics and microbiome-targeted interventions for depression demonstrate modest but measurable improvements in depressive symptoms in some individuals, supporting the concept of gut-mediated modulation rather than direct causation [59,60].
6.4 Neurodevelopmental conditions
The relationship between the gut microbiome and autism spectrum disorder (ASD) has been one of the most intensively studied areas in gut–brain research.
Gastrointestinal symptoms are highly prevalent in individuals with ASD, and multiple studies report distinct microbiome profiles in affected individuals compared with neurotypical controls [5,46,49].
Clostridial species and metabolites have received particular attention. Elevated levels of phenolic compounds such as p-cresol have been reported in subsets of individuals with ASD and are hypothesised to influence neurodevelopment through dopaminergic and inflammatory pathways [11,45,46]. Animal models demonstrate that early-life exposure to propionate or p-cresol can induce behavioural changes resembling core ASD features [45,48].
Interventional studies, including microbiota transfer protocols, have reported sustained improvements in gastrointestinal symptoms and modest improvements in behavioural measures in open-label designs [6,7,50]. While these findings support biological plausibility, they do not establish causality and should be interpreted cautiously [46,50].
Evidence linking Candida to neurodevelopmental conditions is more limited. Current data suggest that fungal dysbiosis may modify symptom expression through immune and metabolic pathways rather than act as a primary driver of neurodevelopmental differences [12,35].
6.5 Neuroinflammation, ageing, and cognitive decline
Chronic low-grade inflammation—sometimes referred to as “inflammaging”—is increasingly implicated in age-related cognitive decline and neurodegenerative disease [21,43,61].
Ageing is associated with changes in gut microbiome composition, reduced barrier integrity, and heightened immune activation, all of which may influence brain health [21,61].
Experimental studies demonstrate that gut-derived inflammatory signals can prime microglia toward a pro-inflammatory phenotype, impairing synaptic function and cognitive performance [43,47,61].
While Candida and Clostridia are not primary causes of neurodegeneration, their contribution to systemic inflammation and metabolic stress may be clinically relevant in older adults and medically vulnerable populations [21,43].
6.6 Clinical synthesis
Taken together, current evidence supports a model in which Candida and Clostridia function as modulators of neuropsychiatric vulnerability rather than deterministic causes of mental illness. Their impact on brain health appears to depend on:
Host susceptibility (genetics, immune status, stress exposure)
Integrity of the intestinal barrier
Overall microbial diversity and metabolic balance
Timing of exposure, particularly during development or ageing
This nuanced framework aligns with contemporary neuropsychiatric research and underscores the importance of integrative, systems-based approaches to mental and cognitive health [1,3,52].
7. Clinical assessment and diagnostic considerations
From a Harvard Health / Cleveland Clinic perspective, evaluation of Candida or Clostridial involvement in neuropsychiatric symptoms should be selective, hypothesis-driven, and integrated into a comprehensive medical assessment. These organisms are rarely the sole explanation for cognitive or mood symptoms and should be considered potential contributors rather than primary causes in most cases [1,9,12].
7.1 When to consider gut dysbiosis clinically
Assessment of gut dysbiosis may be appropriate when neuropsychiatric or cognitive symptoms coexist with one or more of the following features:
Persistent or unexplained gastrointestinal symptoms (bloating, abdominal pain, diarrhoea, constipation, reflux) [12,46]
Symptom onset or exacerbation following antibiotic exposure or gastrointestinal infection [26,37]
Recurrent mucocutaneous fungal infections, suggesting altered host–microbe balance [27,29]
Chronic inflammatory, metabolic, or immune-mediated conditions [21,43]
Functional disorders with suboptimal response to standard psychological or pharmacological therapies [52,59]
Routine screening for Candida or Clostridia in asymptomatic individuals is not recommended, as incidental findings are common and may lead to unnecessary antimicrobial exposure and further microbiome disruption [19,21].
7.2 Diagnostic tools: strengths and limitations
Stool testing
PCR-based and toxin assays are appropriate and evidence-based for suspected Clostridioides difficile infection [37,38].
Broader stool microbiome panels may identify dysbiosis patterns, but reference ranges remain imperfect, and findings should be interpreted in clinical context rather than as standalone diagnoses [19,46].
Organic acid testing
Urinary organic acids such as D-arabinitol (associated with yeast metabolism) and HPHPA (linked to Clostridial metabolism) are sometimes used as indirect markers of microbial activity [35,46].
These markers may support a clinical hypothesis but do not establish causality and should not independently drive treatment decisions [12,35].
Blood markers
Inflammatory markers (e.g. CRP), metabolic parameters, and micronutrient status may provide contextual information regarding immune activation and physiological resilience [21,52].
Candida antibody testing reflects immune exposure rather than active intestinal overgrowth and has limited diagnostic specificity [29].
Overall, diagnostic testing should be viewed as adjunctive, supporting a coherent clinical pattern rather than replacing careful history-taking and examination [1,12].
8. Treatment approaches: an evidence-informed framework
Management of suspected Candida- or Clostridia-related contributions to brain symptoms should prioritise proportionality, safety, and restoration of gut resilience, rather than aggressive microbial eradication [19,21].
8.1 Treating established infection
Confirmed C. difficile infection should be managed according to infectious disease guidelines, with fidaxomicin or vancomycin as first-line therapy depending on clinical context [37,38].
Recurrent C. difficile may warrant consideration of fecal microbiota–based therapies in appropriately selected patients [38,42].
Proven mucocutaneous or systemic candidiasis should be treated with standard antifungal therapy following established clinical protocols [27,29].
These scenarios are distinct from nonspecific symptoms attributed to “overgrowth” without objective evidence of infection.
8.2 Restoring microbial balance and gut function
For individuals with functional gut–brain axis symptoms, foundational strategies supported by current evidence include:
Dietary optimisation, emphasising fibre diversity, whole foods, and reduced ultra-processed food intake [16,21,59]
Targeted prebiotics and probiotics, recognising strain-specific effects and modest effect sizes [59,60]
Support of intestinal barrier integrity through inflammation reduction and nutritional adequacy [21,30]
Stress regulation, sleep optimisation, and physical activity to support vagal tone and HPA-axis balance [10,11,55]
These interventions align with broader recommendations for cardiometabolic and mental health and carry relatively low risk when appropriately individualised [21,52].
+ References
Cryan JF, O’Riordan KJ, Cowan CSM, et al. The microbiota–gut–brain axis. Physiol Rev. 2019;99(4):1877–2013. doi:10.1152/physrev.00018.2018
Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. Annu Rev Med. 2015;66:381–397. doi:10.1146/annurev-med-060513-093958
Dinan TG, Cryan JF. Gut instincts: microbiota as a key regulator of brain development, ageing and neurodegeneration. J Physiol. 2017;595(2):489–503.
Foster JA, McVey Neufeld KA. Gut–brain axis: how the microbiome influences anxiety and depression. Trends Neurosci. 2013;36(5):305–312.
Finegold SM, Dowd SE, Gontcharova V, et al. Pyrosequencing study of fecal microflora of autistic and control children. Anaerobe. 2010;16(4):444–453.
Kang DW, Adams JB, Gregory AC, et al. Microbiota transfer therapy alters gut ecosystem and improves GI and autism symptoms. Sci Rep. 2017;7:406–421.
Kang DW, Adams JB, Coleman DM, et al. Long-term benefit of microbiota transfer therapy. Sci Rep. 2019;9:5821.
Johnson S, Lavergne V, Skinner AM, et al. Clinical practice guideline for Clostridioides difficile infection. Clin Infect Dis. 2021;73(5):e1029–e1044.
Sharon G, Sampson TR, Geschwind DH, Mazmanian SK. The central nervous system and the gut microbiome. Cell. 2016;167(4):915–932.
Smith PA. The tantalizing links between gut microbes and the brain. Nature. 2015;526(7573):312–314.
Pascucci T, Colamartino M, Fiori E, et al. P-cresol alters brain dopamine metabolism and behaviour. Brain. 2020;143(6):e45.
Severance EG, Yolken RH. Fungal antibodies and cognitive function. Schizophr Res. 2012;140(1–3):121–127.
Hsiao EY, McBride SW, Hsien S, et al. Microbiota modulate behavioural and physiological abnormalities. Cell. 2013;155(7):1451–1463.
Sampson TR, Mazmanian SK. Control of brain development by the microbiome. Cell Host Microbe. 2015;17(5):565–576.
Kelly JR, Borre Y, O’Brien C, et al. Transferring depression via the gut microbiota. J Psychiatr Res. 2016;82:109–118.
Silva YP, Bernardi A, Frozza RL. Short-chain fatty acids and brain function. Front Endocrinol. 2020;11: 28.
O’Riordan KJ, Collins MK, Moloney GM, et al. Short chain fatty acids: microbial metabolites for gut–brain communication. Neurosci Biobehav Rev. 2022;134:104–115.
Dalile B, Van Oudenhove L, Vervliet B, Verbeke K. The role of SCFAs in microbiota–gut–brain communication. Nat Rev Gastroenterol Hepatol. 2019;16(8):461–478.
Lopetuso LR, Scaldaferri F, Petito V, Gasbarrini A. Commensal Clostridia and gut homeostasis. Gut. 2013;62(5):759–767.
Atarashi K, Tanoue T, Oshima K, et al. Induction of colonic regulatory T cells by indigenous Clostridium species. Science. 2011;331(6015):337–341.
Thaiss CA, Zmora N, Levy M, Elinav E. The microbiome and innate immunity. Nature. 2016;535:65–74.
Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012;10:735–742.
Iliev ID, Leonardi I. Fungal dysbiosis: immunity and interactions. Nat Rev Immunol. 2017;17(10):635–646.
Hoarau G, Mukherjee PK, Gower-Rousseau C, et al. Bacteriome and mycobiome interactions. Gut. 2016;65(9):1462–1472.
Moyes DL, Wilson D, Richardson JP, et al. Candidalysin is a fungal peptide toxin. Nature. 2016;532:64–68.
Buffie CG, Pamer EG. Microbiota-mediated colonization resistance. Nat Rev Immunol. 2013;13:790–801.
Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for candidiasis. Clin Infect Dis. 2016;62(4):e1–e50.
Dethlefsen L, Relman DA. Antibiotics and the human microbiome. Proc Natl Acad Sci USA. 2011;108(Suppl 1):4554–4561.
Lionakis MS. New insights into host defence against Candida. Nat Rev Immunol. 2014;14:556–564.
Naglik JR, König A, Hube B, Gaffen SL. Candida–epithelial interactions. Nat Rev Microbiol. 2017;15(12):735–748.
Tetel MJ, de Vries GJ, Melcangi RC, et al. Steroids, stress, and the brain. Nat Rev Neurosci. 2018;19:93–104.
Brown GD, Denning DW, Gow NA, et al. Hidden killers: fungal infections. Sci Transl Med. 2012;4(165):165rv13.
Kelly JR, Minuto C, Cryan JF, Clarke G, Dinan TG. Cross-talk between microbiota and blood–brain barrier. Neurogastroenterol Motil. 2015;27(7):1059–1071.
Quigley EMM. Leaky gut—concept or clinical entity? Curr Opin Gastroenterol. 2016;32(2):74–79.
Morris G, Berk M, Carvalho AF, et al. Inflammation and cognition. Prog Neuropsychopharmacol Biol Psychiatry. 2018;83:68–80.
Zimatkin SM, Deitrich RA. Ethanol metabolism in the brain. Alcohol Alcohol. 1997;32(4):379–387.
Leffler DA, Lamont JT. Clostridioides difficile infection. N Engl J Med. 2015;372:1539–1548.
Feuerstadt P, Aroniadis OC, Sokol H, et al. Fecal microbiota products for recurrent C. difficile. N Engl J Med. 2022;386:220–229.
Popoff MR, Bouvet P. Genetic characteristics of Clostridium botulinum toxins. Toxicon. 2013;75:63–89.
Markey L, Hooper A, Melon LC, et al. Gut Candida albicans affects anxiety-like behaviour via endocannabinoids. Cell Rep. 2020;31(4):107–151.
Perry VH, Holmes C. Microglial priming in neurodegenerative disease. Nat Rev Neurol. 2014;10:217–224.
AGA Clinical Practice Update on fecal microbiota–based therapies. Gastroenterology. 2024.
Heneka MT, McManus RM, Latz E. Inflammasome signalling in the CNS. Nat Rev Neurosci. 2018;19:610–621.
Morris G, Maes M. Mitochondrial dysfunction in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2014;48:3–13.
MacFabe DF. Short-chain fatty acid metabolism and autism. Microb Ecol Health Dis. 2012;23:19260.
Vuong HE, Hsiao EY. Emerging roles for the gut microbiome in autism. Biol Psychiatry. 2017;81(5):411–423.
Erny D, Hrabe de Angelis AL, Jaitin D, et al. Host microbiota constantly control maturation of microglia. Nat Neurosci. 2015;18:965–977.
Foley KA, Ossenkopp KP, Kavaliers M, MacFabe DF. Pre- and postnatal exposure to propionic acid. Behav Brain Res. 2014;259:189–200.
Parracho HMRT, Bingham MO, Gibson GR, McCartney AL. Differences between gut microbiota of autistic and neurotypical children. J Med Microbiol. 2005;54:987–991.
Adams JB, Borody TJ, Kang DW, et al. Gastrointestinal microbiota and ASD. Front Cell Infect Microbiol. 2019;9:222.
Sato J, Kanazawa A, Ikeda F, et al. Gut dysbiosis and cognitive fatigue. Sci Rep. 2014;4:451–459.
Miller AH, Raison CL. The role of inflammation in depression. Nat Rev Immunol. 2016;16:22–34.
Schwarcz R, Stone TW. The kynurenine pathway and the brain. Nat Rev Neurosci. 2012;13:465–477.
Irwin MR. Sleep and inflammation. Nat Rev Immunol. 2019;19:702–715.
Herman JP, McKlveen JM, Ghosal S, et al. Regulation of the HPA axis. Compr Physiol. 2016;6:603–621.
Jiang H, Ling Z, Zhang Y, et al. Altered gut microbiota in anxiety disorders. J Psychiatr Res. 2018;104:45–53.
Rudzki L, Szulc A. Immune–gut–brain axis in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2018;83:64–77.
Haroon E, Raison CL, Miller AH. Psychoneuroimmunology of depression. Nat Rev Psychiatry. 2012;8:234–246.
Ng QX, Peters C, Ho CYX, Lim DY, Yeo WS. Probiotics in depression and anxiety: meta-analysis. Nutr Neurosci. 2018;21(3):169–181.
Sarkar A, Lehto SM, Harty S, et al. Psychobiotics and mental health. Trends Cogn Sci. 2016;20(9):679–692.
Franceschi C, Garagnani P, Parini P, Giuliani C, Santoro A. Inflammaging. Nat Rev Endocrinol. 2018;14:576–590.